Discover how gut health and the trillions of microorganisms in your microbiome can influence the onset and progression of autoimmune diseases, including Hashimoto’s thyroiditis and Graves’ disease. Learn practical steps to nurture a balanced gut and potentially mitigate chronic inflammation and autoimmune flares.
Introduction
Autoimmune diseases can appear baffling, as the body inexplicably turns its defenses inward, targeting its own cells and tissues. Conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), multiple sclerosis (MS), inflammatory bowel disease (IBD), Hashimoto’s thyroiditis, and Graves’ disease are characterized by chronic inflammation and immune system dysfunction. While genetic predispositions and environmental exposures remain crucial pieces of the puzzle, a growing body of research points to a surprising influencer: the gut microbiome.
Deep within your gastrointestinal (GI) tract resides a bustling community of microorganisms—bacteria, fungi, viruses, and more—that can either help regulate your immune system or contribute to its overactivity. This article explores the compelling relationship between gut health and autoimmunity, highlighting how a balanced gut may offer a practical avenue for managing—and potentially preventing—various autoimmune conditions.
Autoimmune Conditions: A Quick Overview
Autoimmune diseases occur when the immune system mistakes the body’s own cells and tissues for foreign invaders. Instead of attacking pathogens, it wages war against joints, organs, nerves, or other structures. The result is persistent inflammation that can lead to pain, swelling, tissue damage, and a wide range of systemic symptoms.
Common Autoimmune Disorders
- Rheumatoid Arthritis (RA): Primarily affects the joints
- Systemic Lupus Erythematosus (SLE): Can impact multiple organs (kidneys, skin, joints, etc.)
- Multiple Sclerosis (MS): Damages the protective sheath around nerves
- Inflammatory Bowel Disease (IBD): Includes Crohn’s disease and ulcerative colitis, resulting in chronic GI inflammation
- Hashimoto’s Thyroiditis: Often leads to hypothyroidism, causing fatigue, weight gain, and intolerance to cold
- Graves’ Disease: A hyperthyroid condition typically marked by weight loss, palpitations, and heat intolerance
Although symptoms vary from one condition to another, chronic inflammation and immune system dysregulation unite these disorders under one umbrella.
The Gut Microbiome: A Hidden Ecosystem
Within your gut lies a vibrant community of trillions of microbes—bacteria, viruses, fungi, and other tiny organisms. Far from being mere passengers, these microscopic residents play multiple vital roles:
- Digestion
- Break down fibers and complex carbohydrates that human enzymes can’t handle alone.
- Immunity
- Train immune cells to distinguish between harmless and harmful microbes, supporting immune tolerance.
- Nutrient Absorption
- Aid in extracting and synthesizing certain vitamins and minerals.
- Defense
- Act as a protective barrier against pathogens that might otherwise infiltrate the bloodstream.
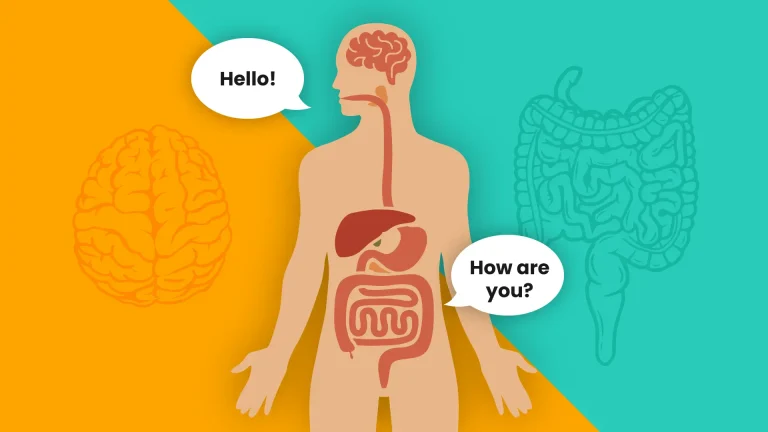
The Gut-Immune Connection: Why It Matters
A well-balanced gut microbiome can be your immune system’s best ally, while a disrupted one can inadvertently fan the flames of autoimmunity. Below are three pivotal ways the gut and immune system intersect:
1. Immune Training and Tolerance
Your immune system constantly surveys the environment for possible threats. The gut, teeming with both beneficial and neutral microbes, acts as an early “classroom” for immune cells. When the microbiome is balanced, the immune system learns to tolerate harmless antigens. In a compromised gut environment—due to poor diet, antibiotic overuse, or chronic stress—the immune system may fail to recognize which microbes (or even which tissues) are friendly, inadvertently launching attacks that can contribute to autoimmune conditions, including thyroid disorders like Hashimoto’s and Graves’ disease.
2. Inflammation Regulation
Inflammation is a hallmark of all autoimmune diseases. Certain gut bacteria produce pro-inflammatory molecules, while others generate compounds that help keep inflammation in check. If your gut microbiome tilts toward inflammatory species, it can magnify or even spark autoimmune flares that affect everything from the thyroid gland to your joints and GI tract.
3. Leaky Gut Syndrome
A healthy intestinal lining acts as a tight barrier, allowing only properly digested nutrients to pass into the bloodstream. When this barrier becomes permeable—a condition sometimes called “leaky gut”—larger molecules, toxins, and bacteria can slip through. This triggers an immune response that may exacerbate or even initiate autoimmunity. For thyroid disorders, ongoing immune activation can attack thyroid cells, leading to either hypothyroidism or hyperthyroidism.
Spotlight on Specific Autoimmune Conditions
- Rheumatoid Arthritis (RA)
- Researchers have found connections between intestinal bacteria—particularly Prevotella copri—and RA onset.
- Gut-driven inflammation may escalate joint swelling and pain.
- Systemic Lupus Erythematosus (SLE)
- Notable differences in the gut microbiomes of individuals with lupus suggest a microbial trigger for heightened immune responses.
- Multiple Sclerosis (MS)
- Immune cells mistakenly attack the myelin sheath around nerve fibers.
- Some research indicates that gut flora composition may influence neurological inflammation, fueling MS progression.
- Inflammatory Bowel Disease (IBD)
- Includes Crohn’s disease and ulcerative colitis; both involve chronic GI inflammation linked to gut microbiome imbalances.
- Hashimoto’s Thyroiditis
- An autoimmune disorder targeting the thyroid, typically causing hypothyroidism.
- Disturbed gut flora and increased intestinal permeability may heighten immune attacks on thyroid cells.
- Graves’ Disease
- Characterized by hyperthyroidism due to thyroid overstimulation.
- Microbial imbalances in the gut can contribute to immune dysregulation, impacting thyroid hormone production.
Factors That Shape Your Gut Health
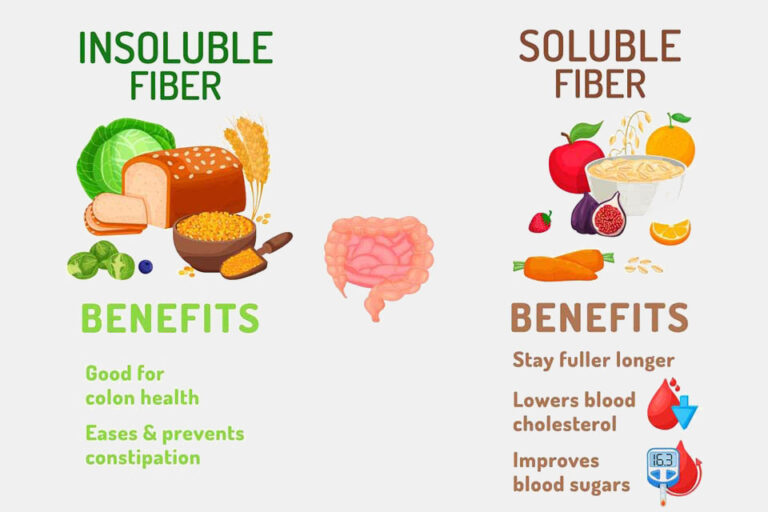
- Diet
- A nutrient-dense, fiber-rich diet encourages beneficial gut bacteria to flourish.
- Fermented Foods (kefir, sauerkraut, kombucha) provide probiotics that may help maintain microbial balance.
- Stress
- Chronic stress disrupts gut harmony, promoting an environment conducive to inflammation.
- Practices like yoga, meditation, or deep breathing can counteract stress-related gut disturbances.
- Medications
- Antibiotics can alter gut bacteria composition—use them only when necessary and replenish beneficial microbes afterward.
- Genetics
- Genetic predispositions exist for many autoimmune disorders, but lifestyle factors can either mitigate or exacerbate disease risk.
- Lifestyle Choices
- Regular Exercise: Moderate physical activity supports a healthy metabolism and beneficial gut flora.
- Sleep: Aim for 7–9 hours to allow for cellular repair and balanced immune function.
Practical Tips to Nurture a Resilient Gut
- Eat a Diverse Diet
- Incorporate fruits, vegetables, whole grains, and legumes.
- Include a variety of fermented foods for probiotic support.
- Manage Stress
- Explore relaxation techniques like guided meditation or mindfulness-based stress reduction.
- Effective stress management can protect against microbiome disruptions.
- Use Antibiotics Wisely
- Only take antibiotics when prescribed by a healthcare provider.
- Consider probiotic supplements to replenish beneficial bacteria.
- Stay Active
- Engage in both aerobic exercise (walking, cycling) and strength training to maintain overall health.
- Physical activity can positively influence gut microbiota diversity.
- Prioritize Quality Sleep
- Consistent, restful sleep is crucial for regulating inflammation and supporting a healthy immune response.
Embracing the Functional Medicine Approach
A functional medicine perspective sees the body as an interconnected system rather than isolated parts. By examining your unique genetics, lifestyle factors, environment, and gut health, a functional medicine practitioner can help reveal the root causes of autoimmunity—beyond merely alleviating symptoms. This approach aims to:
- Identify Underlying Triggers (food sensitivities, infections, toxin exposures)
- Customize Interventions (nutritional therapy, stress management, targeted supplements)
- Promote Sustainable Lifestyle Changes for long-term health benefits
Instead of relying solely on symptom management, functional medicine empowers you to become an active participant in your own healthcare, supporting both your immune system and gut health at the core.
Conclusion: Strengthening Your Gut, Safeguarding Your Thyroid and Beyond
The link between the gut microbiome and autoimmune conditions—including thyroid disorders like Hashimoto’s and Graves’ disease—offers invaluable insights into understanding and managing diseases once considered solely genetic or environmentally driven. By nurturing a balanced microbiome—through a wholesome diet, stress reduction, cautious use of medications, and targeted lifestyle adjustments—you can potentially modulate your immune responses and mitigate chronic inflammation.
Autoimmune disorders can be complex, but actively supporting gut health may lay a foundation for improved vitality and quality of life. Whether you’re seeking to control existing symptoms or prevent future autoimmune flare-ups, investing in a healthy gut is a powerful, proactive step on your journey to wellness.
References
- Belkaid Y, Harrison OJ. Homeostatic Immunity and the Microbiota. Immunity. 2017;46(4):562–576.
- Cani PD, Jordan BF. Gut microbiota-mediated inflammation in obesity: A link with gastrointestinal cancer. Nat Rev Gastroenterol Hepatol. 2018;15(11):671–682.
- Ochoa-Reparaz J, Mielcarz DW, Ditrio LE. Role of Gut Commensal Microflora in the Development of Experimental Autoimmune Encephalomyelitis. J Immunol. 2009;183(10):6041–6050.
- Wu H-J, Wu E. The role of gut microbiota in immune homeostasis and autoimmunity. Gut Microbes. 2012;3(1):4–14.
- Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14(10):573–584.
- Hooper LV, Macpherson AJ. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol. 2010;10(3):159–169.
- He C, Peng W, Wang X, Huang X. Gut microbiome and hyperthyroidism. Front Cell Infect Microbiol. 2022;12:812517.
- Virili C, Centanni M. Does microbiota composition affect thyroid homeostasis? Endocrine. 2015;49(3):583–587.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional regarding diagnosis, treatment, and lifestyle changes.