Fibromyalgia is a perplexing, chronic condition characterized by widespread musculoskeletal pain, persistent fatigue, and sleep disturbances. Those living with fibromyalgia may also experience a phenomenon often referred to as “fibro fog,” marked by issues with memory, concentration, and general cognitive function.
Despite its prevalence, fibromyalgia remains challenging to diagnose and manage because of its complex, multifaceted nature. As a Functional Medicine practitioner, my focus is on uncovering and addressing the root causes behind this condition—exploring factors such as gut health, mitochondrial function, neurotransmitter balance, and possible food sensitivities. This Fibromyalgia Functional Medicine approach allows us to craft an individualized treatment plan that goes beyond symptom relief to promote lasting wellness.
Key Symptoms in a Fibromyalgia Functional Medicine Approach
- Widespread Pain
Individuals often describe fibromyalgia pain as a persistent, dull ache affecting multiple areas, including the neck, shoulders, back, hips, and limbs. This pain may fluctuate in intensity based on factors like stress, physical activity, or weather changes. - Debilitating Fatigue
Fatigue associated with fibromyalgia is not ordinary tiredness; it persists even after adequate rest. Many patients report waking up as exhausted as when they went to sleep, making daily tasks feel insurmountable. - Sleep Disturbances
Insomnia, frequent awakenings, and non-restorative sleep are common concerns. Unfortunately, lack of high-quality sleep can worsen pain sensitivity, creating a vicious cycle of discomfort and fatigue. - Cognitive Issues (“Fibro Fog”)
Memory lapses, attention difficulties, and slowed mental processing often hamper work performance and daily activities. The mental cloudiness can be as distressing as the physical pain. - Mood Fluctuations
Chronic discomfort and low energy can exacerbate feelings of anxiety and depression, further compounding the physical challenges of fibromyalgia.
Root Causes from a Functional Medicine Standpoint
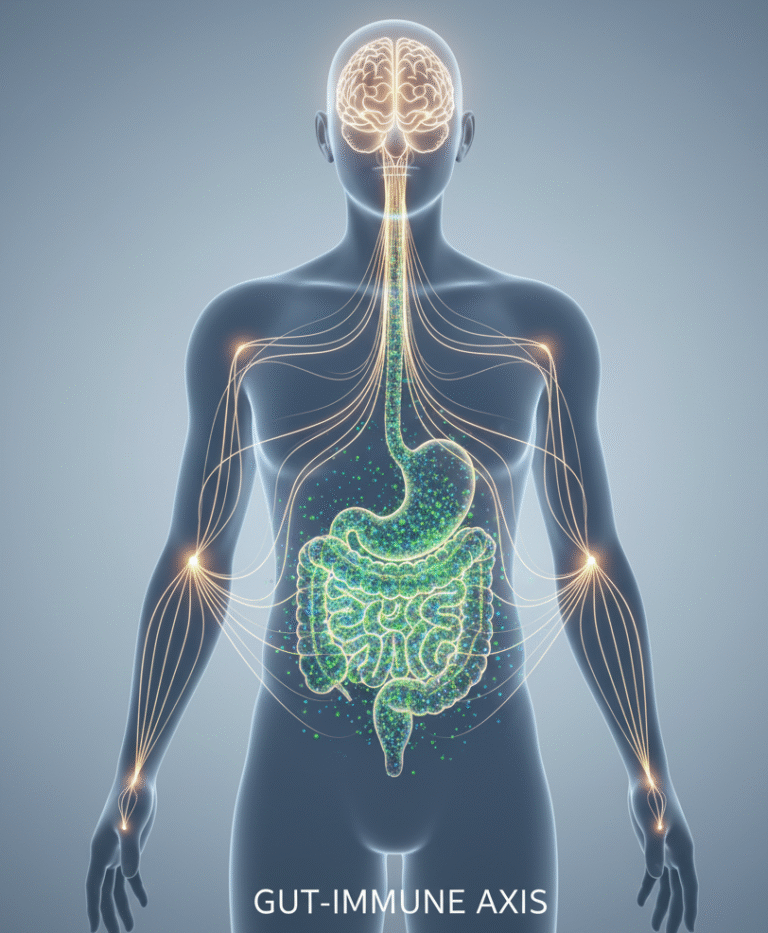
1. Gut Dysbiosis
Emerging research highlights the gut as a pivotal player in fibromyalgia. The gut microbiome, composed of billions of bacteria, influences the immune system and can trigger body-wide inflammation when disrupted. This state of imbalance—known as dysbiosis—may correlate with increased pain and inflammatory markers.
- Impact on Fibromyalgia
Individuals with fibromyalgia often exhibit altered microbial patterns in the gut. These changes can promote systemic inflammation and disrupt the gut-brain axis, potentially intensifying pain perception. - Common Contributing Factors
Antibiotic overuse, diets high in processed foods, chronic stress, and environmental toxins may disrupt the delicate balance of gut flora.
2. Mitochondrial Dysfunction
Mitochondria serve as each cell’s energy powerhouse by generating adenosine triphosphate (ATP). In fibromyalgia, faulty mitochondrial function can diminish ATP production, leading to fatigue and muscle weakness.
- Link to Chronic Fatigue
Reduced energy output may explain why fibromyalgia patients experience profound fatigue after minimal exertion. - Oxidative Stress
When mitochondria struggle to keep up, they often produce excess free radicals. This oxidative stress can intensify pain and inflammation throughout the body.
3. Neurotransmitter Imbalances
Optimal neurotransmitter levels are vital for pain control, mood stability, and overall well-being. Fibromyalgia is frequently associated with irregularities in brain chemicals like serotonin, norepinephrine, dopamine, and substance P.
- Substance P
Elevated substance P can heighten sensitivity to pain, explaining why certain pressure points hurt more in individuals with fibromyalgia. - Serotonin & Norepinephrine
Low levels may contribute to depression and anxiety, while also augmenting the perception of pain.
(Rao et al., “The pharmacology of chronic pain,” Biomedicine & Pharmacotherapy, 2020.)
4. Food Sensitivities
Food intolerances differ from true allergies and can manifest with delayed, subtle symptoms. For fibromyalgia patients, these sensitivities may amplify inflammation and worsen pain or fatigue.
- Common Triggers
Gluten, dairy, corn, soy, and sometimes nightshade vegetables (tomatoes, peppers, potatoes, eggplants) are frequent culprits in many chronic conditions, including fibromyalgia. - The Elimination Diet
Temporarily removing suspect foods and reintroducing them one by one can pinpoint which items provoke flare-ups.
Recommended Testing Approaches
Conventional Testing
- Basic Blood Panels
Doctors generally start with standard blood tests—like a complete blood count (CBC) and thyroid function tests—to rule out other explanations for chronic pain or fatigue (e.g., thyroid disorders, anemia). - Imaging Studies
X-rays or MRIs help exclude issues like arthritis or structural abnormalities but are not definitive for diagnosing fibromyalgia. - Physical Examination
While the older criteria involved tender-point examinations, modern diagnostic methods emphasize a history of widespread pain alongside fatigue, sleep problems, and cognitive symptoms.
Functional Medicine Testing
- Comprehensive Stool Analysis
Provides insight into gut dysbiosis, markers of inflammation, and potential yeast or bacterial overgrowth. - Mitochondrial Function Tests
Evaluates ATP production and oxidative stress, highlighting whether energy metabolism might be compromised. - Neurotransmitter Panels
Measures serotonin, dopamine, norepinephrine, and other neurotransmitters linked to pain regulation and mood. - Food Sensitivity Tests
Assesses delayed hypersensitivity reactions (IgG or IgA), pinpointing triggers that might worsen fibromyalgia symptoms.
Read more: Sugar, Gut Health, and Inflammation: What You Need to Know
Holistic Treatment Strategies in Fibromyalgia Functional Medicine
1. Dietary Interventions
- Anti-Inflammatory Diet
Emphasize whole, nutrient-dense foods rich in antioxidants and omega-3 fatty acids. A diet brimming with leafy greens, colorful vegetables, lean proteins, and healthy fats can help curtail inflammation. - Elimination Protocol
Remove suspect foods for a set period, then systematically reintroduce them. Identifying hidden triggers can bring substantial relief.
2. Nutritional Supplements
- Coenzyme Q10 (CoQ10)
Plays a crucial role in mitochondrial energy production. Research shows that supplementing with CoQ10 may reduce pain and fatigue in fibromyalgia patients. - Magnesium
Essential for muscle relaxation and nerve function. Low magnesium levels have been associated with heightened pain sensitivity. - B-Vitamins
Involved in neurotransmitter synthesis and energy production, especially important for individuals experiencing both fatigue and mood disturbances. - Probiotics
Support a healthy gut microbiome by replenishing beneficial bacteria and combating dysbiosis.
3. Lifestyle Modifications
- Stress Management
Chronic stress amplifies pain. Mindfulness practices, guided meditation, or cognitive-behavioral therapy can help lower cortisol levels and improve coping mechanisms. - Sleep Hygiene
Set a consistent bedtime, keep electronics out of the bedroom, and use calming routines—like gentle stretches or reading—to promote restful sleep. - Physical Activity
While vigorous exercise might worsen symptoms, low-impact activities like swimming, yoga, or tai chi support muscle strength and may ease stiffness without overexertion.
4. Additional Targeted Therapies
- Adaptogenic Herbs
Botanicals like ashwagandha, rhodiola, and holy basil can help rebalance the body’s stress response, potentially mitigating fatigue and tension. - Detoxification Measures
Addressing potential environmental toxins may reduce inflammation and support healthier mitochondrial function. Techniques can include sauna therapy, regular sweating through exercise, and liver-supportive herbs. - Integrative Bodywork
Therapies like massage, acupuncture, or chiropractic adjustments may help release muscle tension, improve circulation, and reduce pain signals.
Read more: Understanding Migraine: Causes, Types, and Modern Treatment Approaches
Looking Ahead: Finding Sustainable Relief
Fibromyalgia is undeniably complex, but that does not mean it’s unbeatable. By investigating root causes—ranging from gut imbalances and mitochondrial glitches to neurotransmitter and food sensitivities—a Functional Medicine approach can reveal the unique blueprint behind each individual’s symptoms. Fibromyalgia Functional Medicine emphasizes this personalized, root-cause strategy. This deep-dive exploration not only informs a more accurate diagnosis but also paves the way for targeted, meaningful interventions.
While conventional medicine provides valuable diagnostic insights, many individuals benefit most when these findings are integrated with functional assessments. With Fibromyalgia Functional Medicine, creating a comprehensive, personalized plan helps us address the systemic imbalances fueling fibromyalgia, rather than merely chasing temporary symptom relief.
If you or someone you know has been struggling with persistent pain, debilitating fatigue, and the frustration of fibro fog, consider exploring Fibromyalgia Functional Medicine. With the right tests and a holistic, root-cause approach, it’s possible to reclaim energy, mobility, and a brighter outlook on life.
References
- Clauw DJ. Fibromyalgia: A Clinical Review. JAMA. 2014;311(15):1547–1555.
- Häuser W, Ablin J, Fitzcharles MA, et al. Fibromyalgia. Nat Rev Dis Primers. 2015;1:15022.
- Farnady C, et al. Gut microbiota composition in individuals with fibromyalgia. Pain. 2022.
- Karperien A, et al. Mitochondrial dysfunction in fibromyalgia. Journal of Pain Research. 2019.
- Rao VV, Mitchell L, Cabot PJ. The pharmacology of chronic pain, mechanism-based therapeutic approaches. Biomedicine & Pharmacotherapy. 2020;132:110.
Disclaimer
The information presented here is intended for educational purposes and should not replace personalized medical advice. If you suspect fibromyalgia or any other chronic condition, please consult a qualified healthcare professional to determine the best plan for your specific needs.