Mitochondria—often called the “powerhouses” of our cells—are central to virtually every aspect of human health. These small, membrane-bound organelles produce adenosine triphosphate (ATP), the chemical energy that fuels our bodies. Beyond powering our cells, mitochondria also play pivotal roles in hormone synthesis, detoxification, and cellular communication. When mitochondrial health is compromised, a wide spectrum of chronic diseases can emerge—from metabolic disorders to neurodegenerative conditions.
In this article, we will explore the fundamentals of mitochondrial function, the various factors that impair mitochondrial health, key diseases linked to mitochondrial dysfunction (including multiple sclerosis under neurodegenerative diseases), reliable testing methods, and a Functional Medicine approach to restoring and optimizing mitochondrial health.
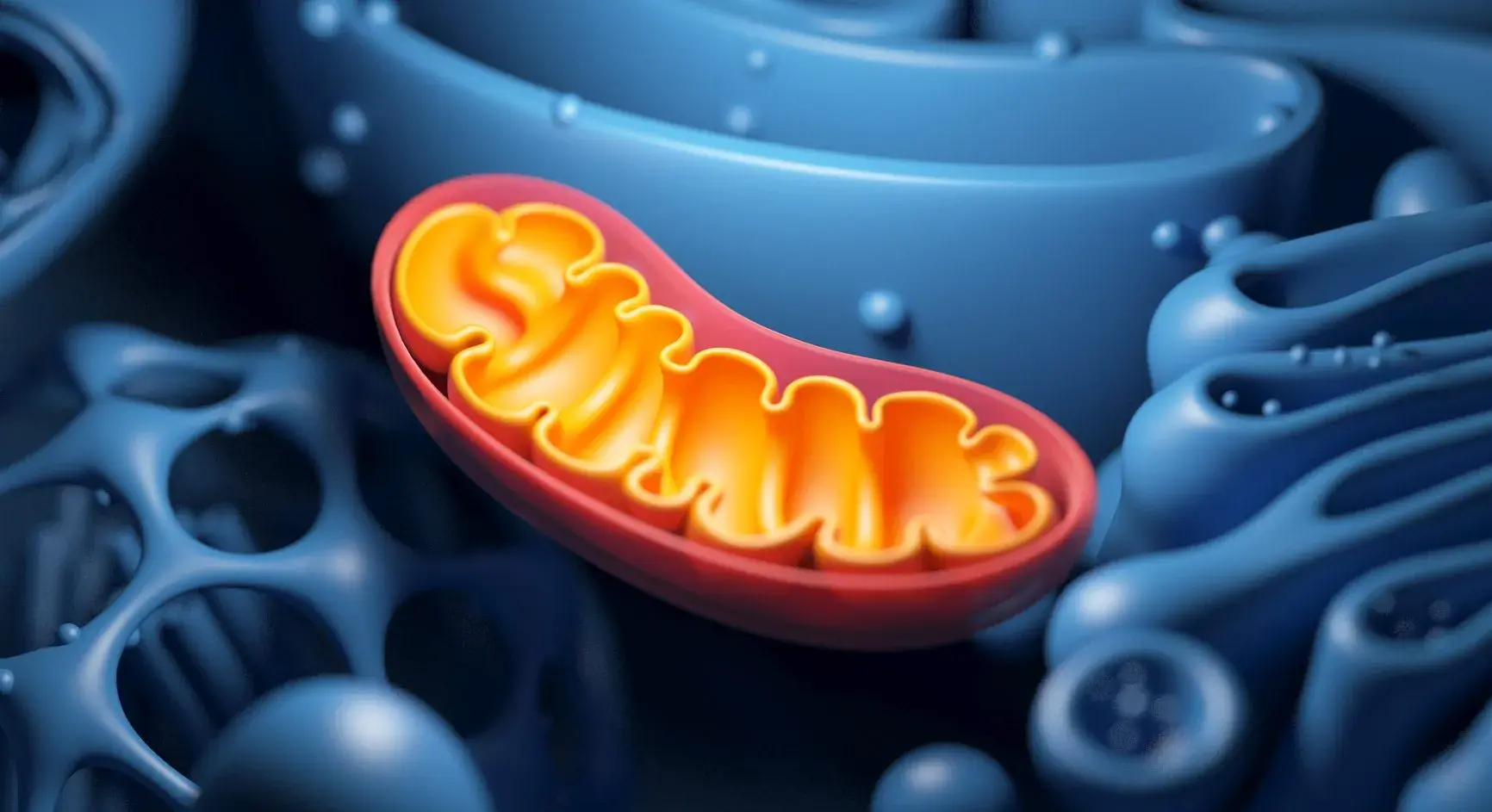
What Are Mitochondria?
Mitochondria are double-membraned organelles found within most human cells. They are chiefly responsible for converting nutrients into ATP via oxidative phosphorylation. However, their influence reaches far beyond energy production:
- Cellular Signaling & Apoptosis
Mitochondria regulate cell growth, coordinate intercellular communication, and govern programmed cell death (apoptosis). - Hormone Synthesis
Mitochondrial pathways are involved in the creation of several key hormones, including certain steroid hormones. - Calcium Homeostasis
Mitochondria help maintain appropriate levels of calcium, essential for muscle contraction, nerve signaling, and more. - Detoxification
By neutralizing reactive oxygen species (ROS) and other byproducts, mitochondria help shield cells from oxidative damage.
Factors That Affect Mitochondrial Health
Several internal and external influences can undermine mitochondrial function:
- Nutrient Deficiencies
- Vitamins (especially B-complex), magnesium, coenzyme Q10 (CoQ10), and alpha-lipoic acid are all crucial for ATP generation.
- Deficits in these micronutrients impair the electron transport chain, compromising cellular energy.
- Exposure to Toxins
- Heavy metals (e.g., mercury, lead) and environmental chemicals (such as pesticides) interfere with mitochondrial enzymes.
- Chronic exposure promotes inflammation and oxidative stress, creating additional strain on energy pathways.
- Chronic Stress
- High cortisol levels and chronic inflammation can disrupt mitochondrial efficiency.
- Stress also impairs nutrient absorption, magnifying mitochondrial damage.
- Poor Sleep & Sedentary Lifestyle
- Inadequate rest deprives the body of essential repair time, weakening mitochondrial recovery processes.
- Lack of exercise stalls mitochondrial biogenesis, leading to reduced ATP production capacity.
- Infections & Immune Dysregulation
- Persistent infections (viral, bacterial, or fungal) can spark ongoing inflammation, harming mitochondria.
- Autoimmune processes heighten oxidative stress, accelerating mitochondrial dysfunction.
Diseases Linked to Mitochondrial Dysfunction
When mitochondria fail to generate adequate energy or suffer structural damage, the downstream effects can be extensive. Key conditions include:
- Chronic Fatigue Syndrome (CFS) & Fibromyalgia
Characterized by relentless fatigue and muscle pain, often tied to insufficient ATP production and heightened oxidative stress. - Neurodegenerative Disorders
Alzheimer’s, Parkinson’s, Huntington’s, and multiple sclerosis (MS) all show evidence of mitochondrial involvement. Neurons rely heavily on constant ATP production, and compromised mitochondria can worsen neurodegeneration through impaired cellular metabolism and elevated ROS. - Metabolic Disorders
Conditions like type 2 diabetes, insulin resistance, and obesity frequently involve mitochondrial dysfunction, given the organelle’s critical role in metabolism. - Cardiovascular Diseases
Heart muscle cells demand a substantial, continuous supply of ATP. Mitochondrial impairment can weaken heart function, contributing to heart failure and other cardiac problems. - Mood & Cognitive Disorders
Depression, anxiety, and cognitive deficits may partially stem from reduced energy availability in neurons and amplified inflammation linked to mitochondrial breakdown.
How to Test for Mitochondrial Dysfunction
Functional Medicine practitioners utilize specialized tests to gauge mitochondrial performance and uncover underlying issues:
- Organic Acids Test (OAT)
Evaluates urinary metabolites that signal nutrient deficiencies and blockages in the electron transport chain. - Comprehensive Nutritional Panels
Measures levels of vitamins, minerals, antioxidants, and cofactors (e.g., CoQ10) vital to mitochondrial health. - Advanced Cardiometabolic Panels
Assesses blood glucose, insulin levels, lipid profiles, and other markers for metabolic dysfunction that stress mitochondria. - Genetic Testing
Identifies gene variants impacting mitochondrial enzymes, detoxification pathways, and nutrient absorption. - Functional Blood Chemistry Analysis
Screens for inflammatory markers such as C-reactive protein (CRP) and homocysteine, giving indirect insights into mitochondrial stress.
Functional Medicine Approach to Treatment
A Functional Medicine protocol seeks to remove stressors, optimize nutrient status, and support the body’s self-healing mechanisms to restore mitochondrial efficiency.
1. Nutritional Optimization
- Anti-Inflammatory Diet
Incorporate whole, nutrient-dense foods, including vibrant fruits and vegetables, lean proteins, and healthy fats like omega-3s. - Targeted Supplementation
B-complex vitamins, magnesium, CoQ10, alpha-lipoic acid, and vitamin D often top the list of essential nutrients for mitochondrial support.
2. Detoxification & Gut Health
- Minimize Toxic Exposures
Limit contact with heavy metals, pesticides, plastics, and other known mitochondrial toxins. - Support Liver Detox
Consume cruciferous vegetables, adequate dietary fiber, and consider supplements like glutathione or N-acetylcysteine to bolster detox pathways. - Foster a Healthy Microbiome
Probiotics and prebiotics help keep systemic inflammation at bay, safeguarding mitochondrial function.
3. Hormonal Balance & Stress Reduction
- Stress Management Tools
Integrate practices such as meditation, yoga, or breathwork to lower cortisol and improve resilience. - Address Endocrine Imbalances
Ensure thyroid, adrenal, and reproductive hormones remain within optimal ranges to sustain steady ATP production.
4. Lifestyle Interventions
- Regular Exercise
Moderate-intensity exercise (e.g., brisk walking, swimming, resistance training) boosts mitochondrial biogenesis and insulin sensitivity. - Adequate Sleep
Aim for 7–9 hours of quality sleep each night for tissue repair, hormone regulation, and toxin clearance. - Sunlight & Red Light Therapy
Natural light exposure or red/infrared therapies can enhance mitochondrial function and support circadian rhythms.
5. Advanced Therapies
- IV Nutrient Therapy
High-dose intravenous vitamins, minerals, and antioxidants can offer rapid replenishment, especially for severe deficiencies. - Peptide Therapy
Emerging research indicates certain peptides may aid in mitochondrial restoration and energy metabolism.
Summary
Mitochondria underpin nearly all biological processes, from muscle movement to cognitive performance. When these vital organelles are compromised by nutrient shortages, environmental toxins, unremitting stress, or immune imbalances, the repercussions can manifest as chronic fatigue, metabolic dysfunction, and a range of neurodegenerative diseases—including multiple sclerosis—under the umbrella of mitochondrial damage. Fortunately, Functional Medicine offers a systematic and individualized path to restoring mitochondrial vitality through precise testing, targeted nutrition, stress management, and other lifestyle interventions.
Take-Home Messages
- Mitochondria Drive Life: They produce ATP but also govern hormone balance, cell signaling, and detoxification.
- Dysfunction Fuels Chronic Illness: Conditions like MS, type 2 diabetes, and cardiovascular disease often have mitochondrial factors at play.
- Testing Matters: Specialized labs—from organic acids to genetic panels—unearth hidden vulnerabilities.
- Lifestyle Changes Are Foundational: An anti-inflammatory diet, regular exercise, stress reduction, and proper sleep can revitalize mitochondrial health.
- Precision Therapies Complement Lifestyle: Targeted supplementation, IV nutrients, and emerging therapies accelerate recovery.
If you suspect that mitochondrial dysfunction is impacting your health—be it through persistent fatigue, hormonal imbalances, or neurological concerns—our Functional Medicine clinic can help. Contact us today to schedule a comprehensive evaluation and begin your personalized journey toward improved energy, mental clarity, and overall vitality.
References
- Mahad D, Ziabreva I, Campbell G, Lassmann H, Turnbull D. Mitochondrial defects in acute multiple sclerosis lesions. Brain. 2008;131:1722–1735.
- Lassmann H. Mitochondrial changes in MS brains: Relevance for the pathogenesis, pathophysiology, and therapy. Curr Opin Neurol. 2017;30(3):239–245.
- Wallace DC. Mitochondrial defects in neurodegenerative and metabolic diseases: A pivotal role of mitochondrial energy metabolism. J Clin Invest. 2013;123(3):1405–1412.
- Myhill S, Booth NE, McLaren-Howard J. Chronic fatigue syndrome and mitochondrial dysfunction. Int J Clin Exp Med. 2009;2(1):1–16.
- Picard M, Juster RP, Madera JJ, et al. Mitochondrial dysfunction and energy deficiency in pathology and aging: Implications for neurodegenerative diseases. Life. 2021;11(8):848.
- Brown GC, Borutaite V. There is no evidence that mitochondria are the main source of reactive oxygen species in mammalian cells. Mitochondrion. 2012;12(1):1–4.
- Croteau D, et al. Mitochondrial disorders: Advances in diagnosis, management, and treatment. Minerva Med. 2017;108(4):320–328.
Disclaimer: This article is intended for informational purposes only and does not replace personalized medical advice. Always consult a qualified healthcare professional for individual evaluation and treatment.