Mycotoxin illness, often referred to simply as “mold toxicity,” is an increasingly recognized condition arising from exposure to harmful fungal byproducts. These toxic compounds—collectively called mycotoxins—can wreak havoc on multiple body systems, triggering chronic inflammation, neurological dysfunction, and hormonal imbalances. Because early signs of mold toxicity frequently overlap with other illnesses, individuals often endure lengthy diagnostic processes before uncovering the true source of their persistent symptoms. A Functional Medicine approach seeks to identify and address these underlying triggers, offering an integrative pathway toward recovery.
Below, we will explore how mycotoxins affect the body, discuss prominent symptoms, outline key diagnostic measures, and present a holistic treatment plan. This article also incorporates insights from cutting-edge research on mold-related disorders, along with practical strategies you can implement to safeguard your health.
Understanding Mycotoxins and Mold Exposure
What Are Mycotoxins?
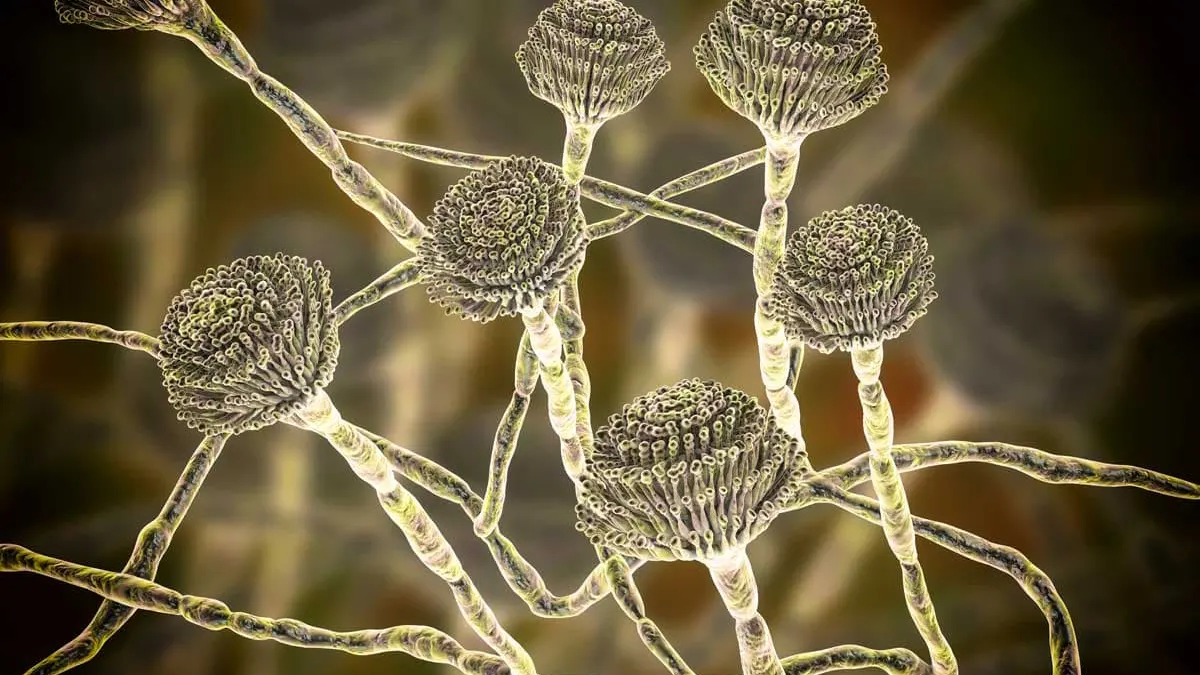
Mycotoxins are secondary metabolites produced by certain molds (fungi), such as Aspergillus, Penicillium, Fusarium, and Stachybotrys. While molds play essential roles in the ecosystem by breaking down organic matter, certain species produce toxins that pose significant risks to humans and animals. When conditions are warm and damp—like those in water-damaged homes, offices, or other buildings—mold can thrive and release these poisonous compounds into the air or onto surfaces.
Over time, occupants can inhale or ingest mycotoxins, allowing the toxins to enter the bloodstream and spread throughout the body. Certain species produce mycotoxins that are carcinogenic, while others disrupt metabolic processes or immune pathways. Continuous or high-level exposure can exacerbate these harmful effects, leading to a complex constellation of symptoms.
(Bennett & Klich, 2003. Clin Microbiol Rev.)
Common Sources of Exposure
- Indoor Environments: Water damage in walls, HVAC systems, carpets, and basements often fosters mold growth.
- Contaminated Food: Stored grains, nuts, coffee beans, and spices can harbor mold that secretes mycotoxins (e.g., aflatoxins in peanuts).
- Occupational Settings: Farms, industrial warehouses, or poorly ventilated workplaces may expose employees to elevated spore counts.
Signs and Symptoms of Mycotoxin Illness
Mycotoxin illness presents with a broad spectrum of symptoms, frequently mirroring other chronic conditions. This overlap can complicate diagnosis and prolong suffering. Commonly reported complaints include:
- Chronic Fatigue
Persistent fatigue unrelieved by rest is often the hallmark of mold toxicity, impacting daily function and overall well-being. - Brain Fog and Cognitive Impairment
Individuals may experience difficulty concentrating, poor memory, or slowed mental processing, sometimes with accompanying mood fluctuations. - Respiratory Issues
Sinus congestion, shortness of breath, asthma-like symptoms, and chronic cough can all stem from inhalation of mold spores or toxins. - Gastrointestinal Disturbances
Some report bloating, abdominal pain, and irregular bowel movements, suggesting that mycotoxins may disrupt the gut microbiome and intestinal barrier integrity. - Skin Problems
Rashes, itching, hives, or increased skin sensitivity may occur in response to mold exposure. - Inflammatory and Immune Dysregulation
Joint stiffness, muscle pain, and recurrent infections point toward underlying inflammatory pathways that mold toxins can exacerbate.
Because these symptoms are diverse and often emerge gradually, individuals may initially attribute them to stress, aging, or unrelated health issues. Recognizing a pattern of symptoms that intensifies when in damp or moldy environments can be a clue pointing toward mold toxicity.
Pathophysiology: Insights from Pioneering Work
Research on the pathophysiological mechanisms of mycotoxin illness has expanded significantly, revealing intricate interactions between fungal toxins and various bodily systems. As described by Dr. Ritchie Shoemaker and Dr. Neil Nathan, mold-triggered inflammation can become chronic, generating a cycle of immune dysregulation and amplified sensitivity to environmental stressors. These toxins may cross the blood-brain barrier, contribute to leaky gut syndrome, disrupt neurotransmitter balance, and impair mitochondrial function—all of which can fuel lingering fatigue, neurological complaints, and systemic inflammation.
(Shoemaker RC, Surviving Mold, 2010; Nathan N, Toxic, 2018.)
Immune System Overload
Mycotoxins can act as persistent antigens, continually activating the immune system. Elevated inflammatory cytokines, such as IL-6 or TNF-α, can exacerbate fatigue and pain. Over time, this heightened immune response may exhaust key regulatory pathways, leading to recurring infections or susceptibility to co-infections (e.g., Lyme disease).
Neurological Disruption
Certain mycotoxins are neurotoxic, impacting synaptic transmission, neurotransmitter levels, and the formation of free radicals in brain tissue. These effects often present as cognitive dysfunction (“brain fog”), mood swings, and even sleep disturbances.
Hormonal and Metabolic Imbalances
Chronic inflammation can hijack the hypothalamic-pituitary-adrenal (HPA) axis, altering cortisol release and straining adrenal function. Thyroid hormones may also be affected, contributing to unrelenting fatigue and sluggish metabolism. In addition, mycotoxins can hamper liver detoxification pathways, compromising the body’s ability to metabolize hormones and clear other toxins.
(Simpson et al., 2016. Toxicology Letters.)
Diagnostic Approaches
Because mold toxicity can mimic numerous chronic illnesses, a thorough evaluation is essential. The following strategies are frequently used by Functional Medicine practitioners:
- Detailed History and Exposure Assessment
A targeted questionnaire examining past or current exposure to water-damaged buildings, occupational hazards, or diets high in potentially moldy foods can provide valuable context. - Environmental Testing
Air sampling, surface swabs, and professional inspections identify mold species and gauge spore counts in a home or workplace. - Laboratory Analyses
- Mycotoxin Panels: Urine or blood testing can detect specific toxins like ochratoxin A, aflatoxins, or trichothecenes.
- Immune Markers: Measures of C4a, TGF-β1, and other inflammatory indicators help assess the severity of the immune response.
- Hormone and Neurotransmitter Panels: Assays for cortisol, thyroid hormones, and neurotransmitter metabolites can reveal physiologic imbalances tied to mold exposure.
- Symptom Scoring and Visual Contrast Sensitivity (VCS) Testing
VCS tests and symptom-based scoring systems can offer additional data points, especially in patients suspected of biotoxin exposure.
Functional Medicine Treatment Framework
1. Remove or Remediate Mold Exposure
Eliminating ongoing contact with mold is critical. This may require professional remediation of water-damaged structures, improving ventilation, and reducing indoor humidity. In extreme cases, relocating or discarding contaminated belongings could be necessary to break the cycle of re-exposure.
2. Support Detoxification Pathways
Clearing toxins from the body involves mobilizing and binding them for excretion:
- Binders: Cholestyramine, activated charcoal, and clay-based binders can help trap mycotoxins in the gut.
- Liver Support: Nutrients like glutathione, N-acetylcysteine (NAC), and milk thistle aid hepatic detoxification processes.
- Hydration: Staying well-hydrated facilitates kidney function and helps flush out circulating toxins.
3. Reduce Inflammation and Oxidative Stress
Chronic inflammation requires a multi-pronged approach:
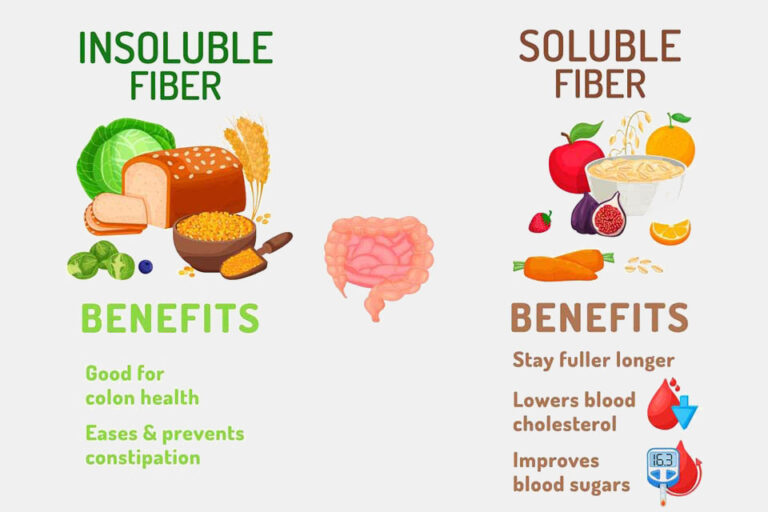
- Anti-Inflammatory Diet: Emphasize whole foods rich in antioxidants, omega-3 fatty acids (from fish oil or algae), and phytonutrients.
- Targeted Supplements: Curcumin, resveratrol, and boswellia can help modulate key inflammatory pathways.
- Lifestyle Measures: Gentle exercise, adequate rest, and stress-reduction techniques (yoga, meditation, breathing exercises) contribute to lowering inflammation.
4. Repair Gut Integrity and Microbiome Balance
Since mycotoxins often disrupt the gut lining, a focus on rebuilding gastrointestinal health is crucial:
- Probiotics and Prebiotics: Restoring beneficial gut flora helps compete against opportunistic microbes.
- Nutrients for Gut Lining: L-glutamine, zinc carnosine, and aloe vera can soothe and repair intestinal permeability.
- Elimination Diet: Identifying and removing problematic foods (gluten, dairy, etc.) may reduce additional inflammatory triggers.
5. Address Hormonal and Neurological Imbalances
Hormones and neurotransmitters may need fine-tuning:
- Adrenal Support: Adaptogenic herbs (ashwagandha, rhodiola) and key vitamins (B5, B6) help restore proper cortisol rhythms.
- Thyroid Assessment: Correcting suboptimal thyroid levels can improve energy and metabolism.
- Cognitive Rehabilitation: Nutrients like phosphatidylserine, acetyl-L-carnitine, or alpha-GPC may help counteract brain fog and enhance mental clarity.
Long-Term Management and Recovery
Regaining full health after mycotoxin illness can be a gradual, multi-stage process. Persistent inflammation and endocrine dysregulation may take time to resolve. Regular follow-ups with a healthcare practitioner experienced in mold toxicity ensure that treatments remain aligned with the patient’s evolving needs.
Moreover, adopting preventive measures can guard against recurrence:
- Maintain Low Indoor Humidity: Ideally, keep levels below 50% to deter mold growth.
- Improve Ventilation: Proper airflow in bathrooms, kitchens, and basements helps limit excess moisture.
- Monitor for Water Damage: Promptly repair leaks in roofs, pipes, or appliances to prevent mold-friendly conditions.
While the road to recovery can be lengthy, many individuals experience significant improvement once they remove ongoing mold exposure, adopt a supportive diet and lifestyle, and implement targeted supplementation. Reclaiming a sense of vitality often means systematically addressing every layer of dysfunction: the environment, detoxification processes, inflammatory cascades, and hormone or neurotransmitter imbalances.
References
- Bennett JW, Klich M. Mycotoxins. Clin Microbiol Rev. 2003;16(3):497–516.
- Shoemaker RC. Surviving Mold: Life in the Era of Dangerous Buildings. 2010.
- Nathan N. Toxic: Heal Your Body from Mold Toxicity, Lyme Disease, Multiple Chemical Sensitivities, and Chronic Environmental Illness. Victory Belt Publishing, 2018.
- Simpson AD, et al. Neurological and behavioral sequelae associated with mycotoxin exposure. Toxicology Letters. 2016;246:77–83.
Disclaimer
This article is provided for informational purposes only. It does not substitute professional medical advice, diagnosis, or treatment. If you suspect mycotoxin illness or have ongoing health concerns, consult a qualified healthcare provider—particularly one familiar with Functional Medicine—to devise a personalized plan tailored to your specific needs.