Are you tired of feeling “off”? In my Oakville functional medicine clinic, I’m seeing a familiar pattern every day: people—especially women and teenagers—struggling with a baffling mix of symptoms. It starts with a little bloating and brain fog, then escalates to nagging joint pain, headaches, skin flares, and a fatigue that no amount of sleep can fix. For some, it’s a diagnosed autoimmune condition; for many others, it’s a frustrating “gray zone” of chronic gut-driven inflammation.
The key insight I want to share with you today is this: your gut and your immune system are in a constant, delicate conversation. What you eat can either soothe that dialogue or turn up the inflammatory volume. As a functional medicine doctor, my mission is to help you uncover the root causes of inflammation, so you can build a life that prevents future flares, rather than simply reacting to them.
Understanding the Autoimmune Puzzle
Autoimmunity is a case of mistaken identity. It happens when your immune system, designed to protect you, mistakenly attacks your own healthy tissues. It’s not a single disease, but a family of conditions that can affect nearly every part of your body.
Some of the most common autoimmune conditions in Canada include:
- Hashimoto’s thyroiditis (thyroid)
- Rheumatoid arthritis (joints)
- Type 1 diabetes (pancreas)
- Celiac disease (small intestine)
- Lupus (connective tissue)
- Psoriasis (skin)
- Inflammatory bowel disease (IBD), including Crohn’s and ulcerative colitis
These aren’t just rare diagnoses. They’re a growing reality for Canadian families. For example, the number of Canadians living with IBD is projected to rise from ~322,600 to nearly 470,000 by 2035. Rheumatoid arthritis affects hundreds of thousands, with a disproportionate impact on women. These are our friends, our family members, our neighbours—and they deserve answers that go beyond just managing symptoms.
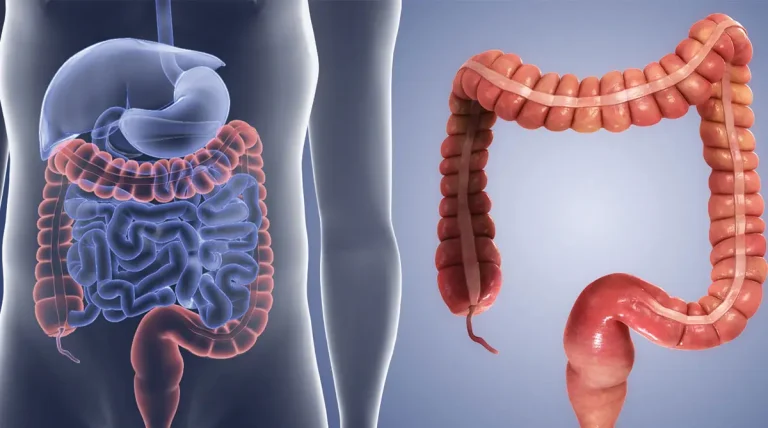
“Leaky Gut” Explained: The Gut-Immune Connection
Your gut lining is a superhero barrier. Just one cell thick, it’s held together by special “tight junctions” that act like a bouncer at a club: they let the good stuff (nutrients) in, while keeping the troublemakers (undigested food particles, microbes) out.
When this barrier becomes more permeable—a condition often called “leaky gut“ or increased intestinal permeability—the bouncer falls asleep on the job. Undigested food proteins and microbial by-products slip into your bloodstream, and your immune system goes into overdrive, triggering the inflammatory cascades that lead to systemic symptoms.
Think of it this way:
- A strong gut barrier means your body is less likely to see everyday foods as a threat.
- A compromised gut barrier creates a vicious cycle: it increases your food sensitivities, and those same reactive foods further damage the barrier. Breaking this loop is the first step toward long-term gut healing.
Food Reactions 101: Allergy, Sensitivity, or Intolerance?
The solution starts with knowing what kind of reaction you’re having.
- Allergy (IgE-mediated): This is a rapid, often severe reaction (hives, wheezing, anaphylaxis) that requires immediate medical attention.
- Sensitivity (typically delayed): Symptoms (bloating, brain fog, joint pain) appear hours or even days after eating. It’s not life-threatening, but it can be life-altering.
- Intolerance (non-immune): This is caused by an issue with digestion, like lactose intolerance, which is due to a lack of the enzyme lactase.
Many people who say they have a “food allergy” actually have a sensitivity or intolerance. The distinction matters because it changes the strategy from a “blanket ban” to a targeted investigation.
The Truth About Gluten: Why It’s Not a Simple Story
The debate over gluten is everywhere, but the reality is personal and nuanced. While it’s not a villain for everyone, here’s why it’s a frequent culprit for those with gut inflammation:
- Gliadin & Gut Permeability: In susceptible people, a key gluten protein called gliadin can loosen the tight junctions in your gut lining, making it more permeable.
- Beyond Gluten: Modern wheat contains other triggers, like amylase-trypsin inhibitors (ATIs), which can activate inflammation, and FODMAPs, which are fermentable carbs that often cause bloating and IBS symptoms. In some studies, these fructans—not the gluten—were the real problem.
- Modern vs. Ancient Wheat: The idea that “ancient wheat is always better” isn’t fully supported by science. While some modern varieties have a higher frequency of certain celiac-related epitopes, ancient wheats can also be high in gluten. The real change? We’re eating more refined flour, more vital wheat gluten in processed foods, and baked goods with shorter fermentation times, which means a higher concentration of triggers for sensitive people.
A practical middle path: For those without celiac disease, traditional long-fermentation sourdough can reduce FODMAPs, making wheat easier to tolerate. It’s a useful tool for strategic reintroduction as part of a personalized plan.
From Symptoms to Success: A Patient’s Functional Medicine Story
Meet A.K.—a 17-year-old student and competitive dancer whose passion for movement was slipping away. She came to me struggling with persistent joint pain, brain fog, headaches, and digestive issues. These weren’t just inconveniences; they were derailing her academics, performance, and confidence.
Unlike conventional quick fixes, our focus was on addressing the root cause of inflammation and restoring balance to her whole body.
Step 1: Mapping the Terrain
We began with a comprehensive functional medicine assessment—exploring her health history, stress levels, sleep quality, and diet. We also conducted specialized functional tests, including:
- Food sensitivity testing to identify potential hidden immune triggers
- Comprehensive stool analysis to evaluate microbiome balance, digestion, and gut inflammation
This allowed us to see the bigger picture rather than chasing isolated symptoms.
Step 2: Targeted Elimination
Based on her results, A.K. began a six-week elimination diet where we removed the most likely inflammatory culprits—gluten and dairy—while focusing on nutrient-dense, anti-inflammatory whole foods.
Step 3: Gut Healing Support
To repair her gut barrier and restore balance, we introduced a personalized gut health protocol:
- Probiotics and prebiotics to rebalance the microbiome
- Key nutrients to calm gut inflammation
- Lifestyle guidance around sleep, stress, and recovery
Step 4: Strategic Reintroduction
Foods were carefully reintroduced one at a time. This step was crucial for identifying her unique triggers without unnecessary long-term restrictions.
The Results: Transformation Within Weeks
Within just six weeks, A.K.’s joint pain and bloating disappeared. Her brain fog lifted, and within two months she was back to full dance training—pain-free, energized, and thriving.
Why This Matters
Stories like A.K.’s aren’t miracles. They’re the natural outcome of a whole-person, science-driven approach that combines advanced functional testing with personalized lifestyle medicine. By targeting the root causes of inflammation, we empower patients to reclaim their health, their passions, and their future.
The Unseen Enemy: How Food, Toxins, and Infections Fuel Autoimmunity
As a functional medicine doctor, I’ve seen firsthand how autoimmune conditions are rising at an alarming rate. Families deserve to know the hidden triggers of autoimmunity—from infections and environmental toxins to fast food and processed diets. This section highlights the science, the statistics, and the everyday habits that can either fuel or reduce inflammation.
Rising Rates of Autoimmune and Chronic Conditions: A Call to Action
The numbers are a wake-up call for our communities.
- In Canada: Nearly 1 in 2 Canadians now live with at least one chronic condition. Autoimmune conditions like Crohn’s disease and ulcerative colitis affect ~330,000 Canadians today and are projected to reach nearly 500,000 by 2035.
- In the United States: More than 15 million Americans (4.6%) are living with at least one autoimmune disease.
- Worldwide: Global studies confirm autoimmunity is increasing year after year.
This isn’t just about statistics. It’s about our children and teens. The earlier they learn how lifestyle, diet, and environment impact immunity, the better their chance to prevent future disease. Prevention is possible, but it starts with understanding the triggers.
Beyond Genetics: Other Root Causes of Autoimmunity
Genetics may load the gun, but your environment pulls the trigger.
- Infections as Triggers: Certain infections can “switch on” autoimmunity in genetically susceptible people. For example, Epstein–Barr virus (EBV) is strongly linked to multiple sclerosis. Post-COVID research also shows an increase in autoimmune diagnoses after infection.
- Environmental Exposures and Gut Health: Toxins, poor sleep, low vitamin D, stress, and gut microbiome imbalance all contribute to inflammation. When the gut barrier becomes “leaky,” the immune system is exposed to food proteins and toxins that it mistakes as threats—fueling autoimmune reactions.
Fast Food and Inflammation: Why That Burger Matters
Fast food is engineered to taste amazing—but beneath the flavor lies an inflammatory storm.
- Fried foods cause spikes in inflammatory markers like IL-6 and CRP.
- Trans fats, though banned in many places, are still present in snacks and fried foods worldwide, increasing systemic inflammation.
- Advanced glycation end-products (AGEs) form during high-heat frying, damaging cells and amplifying inflammation.
The Burger & Avocado Study: In one fascinating clinical trial, eating a burger with avocado led to less inflammation and better vascular function than eating the burger alone. This shows that food combinations matter—healthy fats and antioxidants can buffer inflammatory responses.
Processed Foods: What They Really Mean
“Processed” simply means altered, but ultra-processed foods (UPFs)—think packaged snacks, sodas, fast food, and reconstituted meats—are different. They contain additives, refined sugars, and shelf-stabilizing chemicals.
High UPF intake is directly linked to higher inflammation and worse long-term health outcomes.
Refined Sugar: Pouring Gasoline on the Fire
Sugar is not just empty calories—it’s pro-inflammatory fuel for your gut.
- Studies link sugar-sweetened beverages with increased CRP and IL-6 (key inflammatory markers).
- Diets high in added sugar promote insulin resistance, visceral fat, and chronic low-grade inflammation.
- For teens, daily soda or energy drink consumption may silently prime the body for autoimmune risk.
The Functional Medicine Roadmap to a Calmer You
If you’re ready to get off the inflammation rollercoaster, here’s how a functional medicine approach can help:
- Get Clear on Your Triggers. We’ll use the right tests to differentiate between allergies, sensitivities, and intolerances.
- Stabilize Your Gut Barrier. We focus on a diverse, anti-inflammatory diet rich in proteins, healthy fats, and polyphenols. We also prioritize the fundamentals of sleep, stress management, and movement.
- Time-Box Elimination. We start with a 3–6 week trial removing key culprits, all while ensuring your diet is nourishing and satisfying.
- Reintroduce with Intention. The goal isn’t to take foods away forever. We help you find your personal tolerance thresholds, so you can enjoy the broadest diet possible.
- Expand, Don’t Restrict. This process is about building a sustainable lifestyle that supports your immune system and empowers you with knowledge.
This is a proactive approach to prevention. Done right, it doesn’t just relieve your current symptoms; it lowers your risk of future flares by repairing your gut, calming your immune system, and addressing all the upstream drivers.
Chronic disease and autoimmunity are not inevitable. We can, and must, change the trajectory.
- Educate & Empower: Teach kids and teens that their daily food choices directly shape their immune health.
- Simple Swaps: Show them easy changes: swap out fries for fruit, soda for sparkling water with a splash of juice, and a plain burger for one with avocado and a side salad.
- Encourage Awareness: Help them become conscious of how
processed their food is by reading labels and making informed choices.
As functional medicine doctors, we are here to sound the alarm and remind families that with the right knowledge and daily choices, prevention is not just possible—it’s powerful.
Ready to find your clarity?
If you’re tired of feeling confused and limited by your symptoms, let’s work together to uncover your personal triggers and build a sustainable plan to heal.
Disclaimer
The information provided in this article is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. It should not be taken as a substitute for personalized medical advice. Always consult The information provided in this article is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. It should not be taken as a substitute for personalized medical advice. Always consult with a qualified healthcare professional before making changes to your diet, lifestyle, or treatment plan.
Patient stories shared here are illustrative of functional and naturopathic medicine approaches; individual results will vary. with a qualified healthcare professional before making changes to your diet, lifestyle, or treatment plan. Patient stories shared here are illustrative of functional and naturopathic medicine approaches; individual results will vary.
References:
- Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals an association between Epstein–Barr virus infection and multiple sclerosis. Science. 2022;375(6578):296–301.
- Fasano A. Zonulin, regulation of tight junctions, and autoimmune diseases. Annals of the New York Academy of Sciences. 2012;1258(1):25–33.
- Belkaid Y, Hand TW. Role of the microbiota in immunity and inflammation. Cell. 2014;157(1):121–141.
- National Academies of Sciences, Engineering, and Medicine. Guidance on PFAS Exposure, Testing, and Clinical Follow-Up. Washington, DC: The National Academies Press; 2022.
- Crohn’s and Colitis Canada. The Impact of Inflammatory Bowel Disease in Canada 2023: Final Report. Toronto, ON: Crohn’s and Colitis Canada; 2023.
- Lopez-Garcia E, Schulze MB, Meigs JB, et al. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction in women. The Journal of Nutrition. 2005;135(3):562–566.
- Ghanim H, Sia CL, Upadhyay M, et al. Orange juice blunts the proinflammatory effect of a high-fat, high-carbohydrate meal and prevents endotoxin increase and Toll-like receptor expression. The American Journal of Clinical Nutrition. 2010;91(4):940–949.
- Nappo F, Esposito K, Cioffi M, et al. Postprandial endothelial activation during a fat-rich meal is reduced by antioxidant vitamins. Circulation. 2002;106(16):2067–2072.
- Li Z, Wong A, Henning SM, et al. Hass avocado modulates postprandial vascular reactivity and inflammatory responses to a hamburger meal in healthy volunteers. Food & Function. 2013;4(3):384–391.
- Monteiro CA, Cannon G, Levy RB, Moubarac JC, Louzada ML, Jaime PC. Ultra-processed foods: what they are and how to identify them. Public Health Nutrition. 2019;22(5):936–941.
- Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metabolism. 2019;30(1):67–77.e3.
- Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33(11):2477–2483.